

A decade of value-based care
What’s worked, what hasn’t, and how to prepare for what comes next

JULY/August 2025


JULY/August 2025

Chairman’s Letter
A value-based care report card
decade ago, physicians were very happy with Congress — for once. The politicians had, at last, repealed the Sustainable Growth Rate (SGR) model. For those that remember, elected leaders had been playing a
administrative challenges continue to mount, our mission is to deliver timely content that helps you run your practice more effectively so you can focus on what truly matters: patient care.
What’s new this time?
We learned from our first edition. One of the main pieces of feedback we received was that the experience wasn’t great on mobile. We experimented with some new tools and created an Insider experience this time that is responsive to how you choose to engage with the content, whether on a desktop or laptop or your smart phone.
Let us know what you think about the experience. Reach out to Content Vice President Chris Mazzolini at cmazzolini@mjhlifesciences.com with any tips, feedback or opinions. Thanks as always for reading!
Thank you for joining us on this exciting journey. We are committed to delivering top-tier content that helps you adapt and excel. Stay tuned for more insights from Medical Economics Insider, and together, let’s navigate the complexities of modern medicine.
yearly game of chicken in which Medicare reimbursement hung in the balance unless a last-minute fix was tacked onto some legislation, the doc fix, as it came to be known.
In the spring of 2015, with a 21% reimbursement cut looming, Congress passed the Medicare Access and CHIP Reauthorization Act of 2015, which everyone reading this knows as MACRA, a legislation that ended the SGR for good and, most importantly, brought value-based care into Medicare once and for all, for good and ill.
Ten years later is a good time to take stock on what MACRA has meant to physicians, what has gone right and what has gone wrong, and where it will go in the future. For the cover story in our second edition of Medical Economics Insider, we talked with policy leaders about the progress of value-based care and where is headed.
Also in this issue is a deep dive into physician student loans, which as anyone paying attention to the news knows may be changing rapidly. We also have some exclusive survey data on hot button policy issues and some interactive coding tips.
What’s Insider?
Insider is our new premium interactive digital edition designed to provide physicians with the in-depth insights and practical tools needed to thrive in today’s evolving health care landscape. As business and
July/August 2025
Medical Economics Insider

Mike Hennessy Jr., Chairman and
CEO of MJH Life Sciences®


Check out the first Insider: https://indd.adobe.com/view/eebf2b7e-7b34-4371-b69f-4e99479c0cdf

Chairman’s Letter
A value-based care report card
decade ago, physicians were very happy with Congress — for once. The politicians had, at last, repealed the Sustainable Growth Rate (SGR) model. For those that remember,

elected leaders had been playing a yearly game of chicken in which Medicare reimbursement hung in the balance unless a last-minute fix was tacked onto some legislation, the doc fix, as it came to be known.
In the spring of 2015, with a 21% reimbursement cut looming, Congress passed the Medicare Access and CHIP Reauthorization Act of 2015, which everyone reading this knows as MACRA, a legislation that ended the SGR for good and, most importantly, brought value-based care into Medicare once and for all, for good and ill.
Ten years later is a good time to take stock on what MACRA has meant to physicians, what has gone right and what has gone wrong, and where it will go in the future. For the cover story in our second edition of Medical Economics Insider, we talked with policy leaders about the progress of value-based care and where is headed.
Also in this issue is a deep dive into physician student loans, which as anyone paying attention to the news knows may be changing rapidly. We also have some exclusive survey data on hot button policy issues and some interactive coding tips.
What’s Insider?
Insider is our new premium interactive digital edition designed to provide physicians with the in-depth insights and practical tools needed to thrive in today’s evolving health care landscape. As business and administrative challenges continue to mount, our mission is to deliver timely content that helps you run your practice more effectively so you can focus on what truly matters: patient care.
What’s new this time?
We learned from our first edition. One of the main pieces of feedback we received was that the experience wasn’t great on mobile. We experimented with some new tools and created an Insider experience this time that is responsive to how you choose to engage with the content, whether on a desktop or laptop or your smart phone.
Let us know what you think about the experience. Reach out to Content Vice President Chris Mazzolini at cmazzolini@mjhlifesciences.com with any tips, feedback or opinions. Thanks as always for reading!
Thank you for joining us on this exciting journey. We are committed to delivering top-tier content that helps you adapt and excel. Stay tuned for more insights from Medical Economics Insider, and together, let’s navigate the complexities of modern medicine.
Mike Hennessy Jr.,
Chairman and CEO of MJH Life Sciences®
Check out the first Insider: https://indd.adobe.com/view/eebf2b7e-7b34-4371-b69f-4e99479c0cdf


When Lauren Turich, M.D., a hospitalist trained in family medicine, applied for her first job out of residency, she was sure to choose a nonprofit hospital.
Her reason? To stay on track for Public Service Loan Forgiveness (PSLF).
“Student loans have always been something that I realize in the future I’m going to have to be responsible for, so I’ve had to make decisions with that in mind,” she said. “Having a hospital and residency with the special [nonprofit] status, allowing me to work toward that 10-year requirement for PSLF, that was very important.”
PSLF — a federal program that forgives the remaining balance on direct student loans after 10 years of qualifying payments while working full time for a qualifying employer — is considered one of the most powerful repayment strategies available to physicians with federal student debt, but only if they meet all of the requirements.
Although unique, Turich’s experience attending St. James Medical School in the Caribbean, an international institution that does not qualify for federal student aid, largely reflects a new reality. For many physicians, student loan repayment isn’t just a financial issue; it’s a career-defining variable.
Medical education debt affects everything from job selection and geographic mobility to personal milestones like buying a home or starting a family.
Many medical students enter the classroom aware of the looming debt but may not grasp how deeply it will shape their careers. For some, the promise of eventual forgiveness or relief offers a psychological cushion; for others, it means living with uncertainty as political winds shift.
“For many physicians, student loan repayment isn’t just a
financial issue; it’s a career-defining variable.”
That uncertainty has only deepened. Recent challenges to federal repayment plans have thrown key programs into limbo. Income-driven repayment (IDR) options are facing legal threats. A cornerstone forgiveness plan has been frozen by court order. Proposed legislation could retroactively deny loan forgiveness to physicians still in training.
In an environment where regulations can vanish with a singular election or lawsuit, physicians are increasingly forced to build their futures on policies that may not exist in five years — or even next year.
A diploma (and six figures of debt)
According to the American Association of Medical Colleges’ (AAMC) 2024 Graduation Questionnaire, the median education debt among medical school graduates with debt is $207,000, and 71% of 2024 graduates reported having education debt, most of it from federal student loans.
James Dahle, M.D., F.A.C.E.P., founder of The White Coat Investor, put today’s debt burden into perspective. “The average debt that M.D. students are reporting coming out of school is [roughly] $200,000,” Dahle said on an episode of Off the Chart: A Business of Medicine Podcast. “That number hasn’t changed in years, and if you look at the percentage of students that have any student loan debt coming out, it’s dropping.”
This claim is supported by AAMC data, which shows a 5% drop in the percentage of students with education debt compared with 2017.
Kristen Earle, director of student financial services at the AAMC, emphasized the importance of early financial literacy and budgeting.
“We always like to recommend having a sound money management and budgeting strategy as well as an understanding of one’s discretionary income picture,” she said. She also encouraged medical students to assess their future financial picture realistically and early.
“Determining how and when one will be paid, understanding the repayment terms and cost of loans, the importance of maintaining accurate financial records — all of that helps form a long-term strategy,” Earle said.
Navigating the uncertainty of student loans
A guide for physicians
For most physicians, the biggest decision after medical school isn’t where to work or what to practice; it’s how to repay a mountain of debt in a system that’s constantly shifting under their feet

Lauren Turich, M.D., M.P.H., M.S., a family medicine trained hospitalist, offers financial advice for early-career physicians, based on her own experience with student loans, including the “live like a resident” strategy.
The AAMC has also seen a notable uptick in interest in PSLF over the last five years. “The interest from that [AAMC Graduate Questionnaire] survey was 79.3% for PSLF in 2020, and that’s risen all the way to 88.3% for the last year we have data, in 2024,” Earle said.
Factors contributing to recent increases in debt, including the end of the COVID-19 pandemic-era interest pauses, rising living costs, and increases in the price of attendance, are being closely monitored. Still, Earle noted, “After controlling for inflation, medical student debt really has been mostly stable over the past seven years.”
The most important financial decision of their lives
Michael Foley, C.F.P., C.S.L.P., C.K.A., says new doctors often misunderstand just how significant these loans become — and how quickly. As a comprehensive financial adviser with North Star Resource Group in Scottsdale, Arizona, Foley has been advising physicians on student debt for nearly a decade. He says the financial reality for physicians begins with their outsize loan burdens.
“Medical professionals graduate with an exponentially higher loan balance than most. Society expects doctors to come out swinging with big lifestyles, fancy cars, big houses — but not all of them do,” Foley said. “The majority of them fall into this path where student loans are such a big part of their budget that it often impacts what house they can buy and what they’re actually saving for retirement.”
Dahle agreed. “Trust me when I say that you do not want to have these loans at midcareer,” he said. “You don’t want to be 45, 50 or 55 years old and still owe six figures in student loans. … Refinancing helps a little … but the way to get rid of that is mostly just keep your lifestyle down. I call this the ‘live like a resident’ period of your life.”
According to Dahle, even aggressive repayment is preferable to dragging out loans unnecessarily. “You only give yourself a little bit of an increase in your lifestyle, and you send big checks to the lender every month,” he said. “If you send them a check for $8,000, $10,000 or $12,000 a month, your $200,000, $300,000 or $400,000 in student loans will go away very quickly — and then you’re free.”
Physicians often approach Foley with the sense that their loans are already forgiven. “When they’re going for some of these forgiveness programs, they’ve almost written them off in their minds as if they’re already forgiven. They’re not,” Foley said. “Sometimes it takes a re-grounding to understand that, ‘Hey, this is an actual debt that we owe.’”
A common mistake that new doctors make is raising their fixed expenses too quickly after finishing residency. “They come out and buy that big house right out of the gate,” he explained. “Then they have kids, then they have all these new fixed expenses come up, and they feel like they don’t know where their money’s going anymore.”
“Physicians are increasingly forced to build their futures on policies
that may not exist in five years — or even next year.”
Foley said he also sees new physicians accumulate credit card debt as they near the end of their training, with the assumption that future income will erase it. “Oftentimes they do, but it puts almost everything else on hold for another year or two,” he said. “They’re prespending future dollars at a more accelerated pace than they’re actually going to be earning.”
He added that many of his physician clients also forget to factor in taxes when estimating their take-home pay. “They’re going to be making $300,000, so they expect to be making $25,000 a month, but when they actually look at their paycheck and they’re taking home like $12,000, they say, ‘What the heck? Where’s all my money?’”
their annual income, or two times what their income is, that’s when we’re starting to run some of those numbers,” he said. But this strategy requires planning for the so-called tax bomb, that large tax bill in the forgiveness year that can be financially devastating if you are unprepared.
The third path involves tax-free forgiveness programs, the quintessential one being PSLF, which is available after 10 years (120 months) of qualifying payments made while working full time for an eligible employer.
Dahle pointed to PSLF as a surprisingly generous option in recent years. “Tens of thousands of doctors have received basically a tax-free check for $200,000, $300,000 or $400,000,” he explained.
Still, Dahle was blunt about the risks. “As soon as you know you’re not going into a qualifying job, you might as well refinance them and get a lower interest rate,” he said. “Then you’ve got to stamp them out.”
The official studentaid.gov website clarifies that, to qualify for PSLF, you must meet the following criteria:
The most important factor determining whether you qualify for PSLF is the organization you work for, not the kind of work you do. Examples of ineligible employers include for-profit organizations and for-profit contracted organizations, labor unions and partisan political organizations.
“You have to be on an IDR plan,” Foley said. “When that’s forgiven at the 10th year, [instead of the 20th or 25th year], there’s no taxes due on that.” It’s considered the most efficient and generous program but demands precise documentation, long-term nonprofit employment and strategic income reporting.
In some cases, state-based Loan Repayment Assistance Programs or federal programs like the Veterans Administration’s (VA) Education Department Reduction Program can supplement or replace the above strategies. Foley highlighted the VA’s program as a standout.
“It’s a reimbursement plan, so you pay toward your loans, and then they reimburse you that amount. You can do that for five years, all the way up to $200,000,” he said. “It’s kind of a retention program for the VA.” The reimbursements are in addition to potential PSLF eligibility, which makes Foley consider the VA the “golden child.”
Choosing the right path, Foley said, requires assessing income, debt size and job setting. “We always want to look at what the total cost is and compare it to if we were to just pay it off aggressively,” he said, adding that, for some clients, the forgiveness path yields hundreds of thousands in savings. For others, exiting the federal system and attacking the balance head-on is more efficient.
Shifting winds in Washington
Policy changes in Washington, D.C., under the Trump administration have opened the door to additional uncertainty around the future of student loan repayment. Most notably, the SAVE plan, introduced in 2023 as a more generous IDR option, has been tied up in federal court.
In early 2024, two coalitions of Republican-led states filed lawsuits in federal court challenging the SAVE plan, arguing that the Biden administration lacked the authority to overhaul repayment programs unilaterally. Months later, the 8th Circuit Court of Appeals ordered the Department of Education to halt implementation of SAVE while the case proceeds. As a result, borrowers enrolled in SAVE were placed into a general forbearance period, during which interest is paused, but so is progress toward forgiveness.
“They’re going to be making $300,000, so they expect to be making $25,000 a month, but when they actually look at their paycheck and they’re taking home like $12,000, they say, ‘What the heck?
Where’s all my money?’”
Foley cited the situation with the SAVE plan as a reason for physicians to be wary of how quickly regulatory programs can change. He also noted the broader implications of the Supreme Court’s 2024 overturning of the longstanding Chevron doctrine, which gave regulators the power and legal insulation to create regulations under laws without congressional approval. The Chevron doctrine was in play in 2023 when the Biden administration used the Department of Education to roll out the SAVE plan without congressional approval.
James Dahle, M.D., FACEP, founder of The White Coat Investor, says PSLF has been a “game changer” for physicians, with many receiving tax-free relief for hundreds of thousands of dollars. He highlights how programs like SAVE offer unprecedented generosity, even halting loan growth during residency. “Don’t be too fatalistic,” Dahle says — today’s doctors have more repayment options than ever.
“Some of the IDR programs have been incredibly generous, [for example], this one that the Trump administration is doing its best to stamp out,” Dahle said, referring to the SAVE plan. “It was a very, very generous program. … Your debt wasn’t even going up in residency like it used to.”
“A lot of things that we felt like we could count on have been pulled out from underneath us,” Foley said. “With the Chevron doctrine going away, it kind of dismantled the power of the Department of Education’s regulations. We’re at risk of them potentially changing those IDR plans down the line.”
Foley explained that only one IDR plan is rooted in law: IBR. “Plans like PAYE, SAVE, Income-Contingent Repayment, Income-Sensitive — those are regulations that could be sued in the future, just like SAVE is being sued right now.”
The implications stretch beyond legal battles. Under the court-ordered forbearance, no new borrowers can enroll in SAVE, and existing participants are not earning credit toward PSLF or IDR forgiveness unless they switch to IBR. And while IBR remains the only IDR plan currently processing forgiveness, because Congress established it, it may not be the best option for every physician, depending on income, debt load and career path.
At the same time, House Republicans are advancing legislation to cap federal graduate student borrowing at $150,000 and remove PSLF credit for time spent in medical or dental residency. This change could dramatically increase costs for trainees at nonprofit hospitals.
Other Republican-led proposals would limit who qualifies for forgiveness based on the employer’s political or advocacy affiliations, raising further concerns about future restrictions to PSLF.
“There’s also processing risk,” Foley said. “The loan servicers can be very difficult to deal with. … A lot of our clients are in the SAVE plan, and servicers are refusing to process applications to switch to IBR right now. So months go by without any credit toward PSLF or other forgiveness options.”
In an April letter, the American Medical Association (AMA) urged the Trump administration to take action on processing delays, PSLF protections and the broader uncertainty surrounding the status of IDR plans.
“This uncertainty … has caused individuals to experience continued increases in their student loan balance due to constantly accruing interest, a lack of knowledge surrounding payment amounts, and the inability to continue to accumulate time toward loan forgiveness,” wrote James L. Madara, M.D., CEO and executive vice president of the AMA.
Madara warned that instability in PSLF could undercut physician willingness to serve in high-need areas. “If this uncertainty continues … it will impact physicians’ desire to participate and thus will decrease access to much-needed medical care for patients in underserved communities.”
With the Trump administration signaling skepticism toward large-scale loan forgiveness — and key regulatory protections under legal assault — the repayment landscape for physicians has become more uncertain than ever.
Despite that volatility and ongoing legislative upheavals, the financial principles guiding loan repayment remain stable: Physicians must maintain careful, strategic approaches tailored to their individual circumstances.
Dahle remains optimistic. “Let’s not be too fatalistic that student loans are a terrible, terrible problem out there,” he said. “In a lot of ways, a lot has been done on this, and there’s a lot of great options.”
Whether relying on PSLF, pursuing aggressive repayment or navigating long-term forgiveness strategies, ongoing vigilance to policy developments is essential. More than ever, physicians must stay informed and flexible, ready to adapt to the evolving student loan landscape that continues to shape their careers and lives.
Debt-video-3
Videos in this feature
July/August 2025
Medical Economics Insider


Michael Foley, CFP, CSLP, CKA, a comprehensive financial advisor with North Star Resource Group, shares how physicians should balance student loan repayment with saving. He advises covering the basics first — emergency fund, insurance and retirement match — then taking a split approach, paying down loans while building savings in case forgiveness programs fall through.
Debt-video-2
Related Podcast episode
Understanding your options: The three paths
Foley broke down the repayment landscape into three primary options, each with significant trade-offs depending on income, employment type and total debt. “To get rid of people’s student loans, they have to go through one of these three paths,” Foley said.
The first is direct payment. This includes either staying in the federal system and making full monthly payments or refinancing into a private loan and choosing a fixed timeline, typically five, 10 or 15 years. This path offers simplicity and lower total interest costs for physicians with high incomes and relatively lower loan balances.
“We always want to compare the total cost of paying it off versus the forgiveness routes,” Foley explained. If the difference is small, aggressive repayment may be the safer route.
The second option is long-term IDR with taxable forgiveness at the end. Under plans like Income-Based Repayment (IBR), Pay As You Earn (PAYE) or Saving on A Valuable Education (SAVE), monthly payments are based on income and household size, not outstanding loan balance. After 20 to 25 years of monthly payments, the remaining balance is forgiven, but the forgiven amount is treated as taxable income in the year it’s forgiven.
“If you still have a balance remaining at the end of that 20 to 25 years, they’ll say, ‘Hey, you can throw in the towel. We’re going to forgive them for you,” Foley explained, including the caveat that “if you still have $300,000 remaining at that point, they’re going to add that to your taxable income in that final year of distribution. So it’s forgiven, but it’ll look like you just made an extra $300,000 that year.”
Foley described this as a necessary path for borrowers whose debt far exceeds their income, particularly those in lower-paying specialties. “If their loan balance is higher than
When Lauren Turich, M.D., a hospitalist trained in family medicine, applied for her first job out of residency, she was sure to choose a nonprofit hospital.
Her reason? To stay on track for Public Service Loan Forgiveness (PSLF).
“Student loans have always been something that I realize in the future I’m going to have to be responsible for, so I’ve had to make decisions with that in mind,” she said. “Having a hospital and residency with the special [nonprofit] status, allowing me to work toward that 10-year requirement for PSLF, that was very important.”
PSLF — a federal program that forgives the remaining balance on direct student loans after 10 years of qualifying payments while working full time for a qualifying employer — is considered one of the most powerful repayment strategies available to physicians with federal student debt, but only if they meet all of the requirements.
Although unique, Turich’s experience attending St. James Medical School in the Caribbean, an international institution that does not qualify for federal student aid, largely reflects a new reality. For many physicians, student loan repayment isn’t just a financial issue; it’s a career-defining variable.
Medical education debt affects everything from job selection and geographic mobility to personal milestones like buying a home or starting a family.
Many medical students enter the classroom aware of the looming debt but may not grasp how deeply it will shape their careers. For some, the promise of eventual forgiveness or relief offers a psychological cushion; for others, it means living with uncertainty as political winds shift.
“For many physicians, student loan repayment isn’t just a financial issue; it’s a career-defining variable.”
That uncertainty has only deepened. Recent challenges to federal repayment plans have thrown key programs into limbo. Income-driven repayment (IDR) options are facing legal threats. A cornerstone forgiveness plan has been frozen by court order. Proposed legislation could retroactively deny loan forgiveness to physicians still in training.
In an environment where regulations can vanish with a singular election or lawsuit, physicians are increasingly forced to build their futures on policies that may not exist in five years — or even next year.
A diploma (and six figures of debt)
According to the American Association of Medical Colleges’ (AAMC) 2024 Graduation Questionnaire, the median education debt among medical school graduates with debt is $207,000, and 71% of 2024 graduates reported having education debt, most of it from federal student loans.
James Dahle, M.D., F.A.C.E.P., founder of The White Coat Investor, put today’s debt burden into perspective. “The average debt that M.D. students are reporting coming out of school is [roughly] $200,000,” Dahle said on an episode of Off the Chart: A Business of Medicine Podcast. “That number hasn’t changed in years, and if you look at the percentage of students that have any student loan debt coming out, it’s dropping.”
This claim is supported by AAMC data, which shows a 5% drop in the percentage of students with education debt compared with 2017.
Kristen Earle, director of student financial services at the AAMC, emphasized the importance of early financial literacy and budgeting.
“We always like to recommend having a sound money management and budgeting strategy as well as an understanding of one’s discretionary income picture,” she said. She also encouraged medical students to assess their future financial picture realistically and early.
“Determining how and when one will be paid, understanding the repayment terms and cost of loans, the importance of maintaining accurate financial records — all of that helps form a long-term strategy,” Earle said.
For most physicians, the biggest decision after medical school isn’t where to work or what to practice; it’s how to repay a mountain of debt in a system that’s constantly shifting under their feet
By Austin Littrell Assistant editor
Time to read: 11 - 12 minutes
Lauren Turich, M.D., M.P.H., M.S., a family medicine trained hospitalist, offers financial advice for early-career physicians, based on her own experience with student loans, including the “live like a resident” strategy.
Michael Foley, CFP, CSLP, CKA, a comprehensive financial advisor with North Star Resource Group, shares how physicians should balance student loan repayment with saving. He advises covering the basics first — emergency fund, insurance and retirement match — then taking a split approach, paying down loans while building savings in case forgiveness programs fall through.
The AAMC has also seen a notable uptick in interest in PSLF over the last five years. “The interest from that [AAMC Graduate Questionnaire] survey was 79.3% for PSLF in 2020, and that’s risen all the way to 88.3% for the last year we have data, in 2024,” Earle said.
Factors contributing to recent increases in debt, including the end of the COVID-19 pandemic-era interest pauses, rising living costs, and increases in the price of attendance, are being closely monitored. Still, Earle noted, “After controlling for inflation, medical student debt really has been mostly stable over the past seven years.”
The most important financial decision of their lives
Michael Foley, C.F.P., C.S.L.P., C.K.A., says new doctors often misunderstand just how significant these loans become — and how quickly. As a comprehensive financial adviser with North Star Resource Group in Scottsdale, Arizona, Foley has been advising physicians on student debt for nearly a decade. He says the financial reality for physicians begins with their outsize loan burdens.
“Medical professionals graduate with an exponentially higher loan balance than most. Society expects doctors to come out swinging with big lifestyles, fancy cars, big houses — but not all of them do,” Foley said. “The majority of them fall into this path where student loans are such a big part of their budget that it often impacts what house they can buy and what they’re actually saving for retirement.”
Dahle agreed. “Trust me when I say that you do not want to have these loans at midcareer,” he said. “You don’t want to be 45, 50 or 55 years old and still owe six figures in student loans. … Refinancing helps a little … but the way to get rid of that is mostly just keep your lifestyle down. I call this the ‘live like a resident’ period of your life.”
According to Dahle, even aggressive repayment is preferable to dragging out loans unnecessarily. “You only give yourself a little bit of an increase in your lifestyle, and you send big checks to the lender every month,” he said. “If you send them a check for $8,000, $10,000 or $12,000 a month, your $200,000, $300,000 or $400,000 in student loans will go away very quickly — and then you’re free.”
Physicians often approach Foley with the sense that their loans are already forgiven. “When they’re going for some of these forgiveness programs, they’ve almost written them off in their minds as if they’re already forgiven. They’re not,” Foley said. “Sometimes it takes a re-grounding to understand that, ‘Hey, this is an actual debt that we owe.’”
A common mistake that new doctors make is raising their fixed expenses too quickly after finishing residency. “They come out and buy that big house right out of the gate,” he explained. “Then they have kids, then they have all these new fixed expenses come up, and they feel like they don’t know where their money’s going anymore.”
“Physicians are increasingly forced to build their futures on policies
that may not exist in five years — or even next year.”
Foley said he also sees new physicians accumulate credit card debt as they near the end of their training, with the assumption that future income will erase it. “Oftentimes they do, but it puts almost everything else on hold for another year or two,” he said. “They’re prespending future dollars at a more accelerated pace than they’re actually going to be earning.”
He added that many of his physician clients also forget to factor in taxes when estimating their take-home pay. “They’re going to be making $300,000, so they expect to be making $25,000 a month, but when they actually look at their paycheck and they’re taking home like $12,000, they say, ‘What the heck? Where’s all my money?’”
Foley described this as a necessary path for borrowers whose debt far exceeds their income, particularly those in lower-paying specialties. “If their loan balance is higher than their annual income, or two times what their income is, that’s when we’re starting to run some of those numbers,” he said. But this strategy requires planning for the so-called tax bomb, that large tax bill in the forgiveness year that can be financially devastating if you are unprepared.
The third path involves tax-free forgiveness programs, the quintessential one being PSLF, which is available after 10 years (120 months) of qualifying payments made while working full time for an eligible employer.
Dahle pointed to PSLF as a surprisingly generous option in recent years. “Tens of thousands of doctors have received basically a tax-free check for $200,000, $300,000 or $400,000,” he explained.
Still, Dahle was blunt about the risks. “As soon as you know you’re not going into a qualifying job, you might as well refinance them and get a lower interest rate,” he said. “Then you’ve got to stamp them out.”
The official studentaid.gov website clarifies that, to qualify for PSLF, you must meet the following criteria:
The most important factor determining whether you qualify for PSLF is the organization you work for, not the kind of work you do. Examples of ineligible employers include for-profit organizations and for-profit contracted organizations, labor unions and partisan political organizations.
“You have to be on an IDR plan,” Foley said. “When that’s forgiven at the 10th year, [instead of the 20th or 25th year], there’s no taxes due on that.” It’s considered the most efficient and generous program but demands precise documentation, long-term nonprofit employment and strategic income reporting.
In some cases, state-based Loan Repayment Assistance Programs or federal programs like the Veterans Administration’s (VA) Education Department Reduction Program can supplement or replace the above strategies. Foley highlighted the VA’s program as a standout.
“It’s a reimbursement plan, so you pay toward your loans, and then they reimburse you that amount. You can do that for five years, all the way up to $200,000,” he said. “It’s kind of a retention program for the VA.” The reimbursements are in addition to potential PSLF eligibility, which makes Foley consider the VA the “golden child.”
Choosing the right path, Foley said, requires assessing income, debt size and job setting. “We always want to look at what the total cost is and compare it to if we were to just pay it off aggressively,” he said, adding that, for some clients, the forgiveness path yields hundreds of thousands in savings. For others, exiting the federal system and attacking the balance head-on is more efficient.
Shifting winds in Washington
Policy changes in Washington, D.C., under the Trump administration have opened the door to additional uncertainty around the future of student loan repayment. Most notably, the SAVE plan, introduced in 2023 as a more generous IDR option, has been tied up in federal court.
In early 2024, two coalitions of Republican-led states filed lawsuits in federal court challenging the SAVE plan, arguing that the Biden administration lacked the authority to overhaul repayment programs unilaterally. Months later, the 8th Circuit Court of Appeals ordered the Department of Education to halt implementation of SAVE while the case proceeds. As a result, borrowers enrolled in SAVE were placed into a general forbearance period, during which interest is paused, but so is progress toward forgiveness.
“They’re going to be making $300,000, so they expect to be making $25,000 a month, but when they actually look at their paycheck and they’re taking home like $12,000, they say, ‘What the heck? Where’s all my money?’”
Foley cited the situation with the SAVE plan as a reason for physicians to be wary of how quickly regulatory programs can change. He also noted the broader implications of the Supreme Court’s 2024 overturning of the longstanding Chevron doctrine, which gave regulators the power and legal insulation to create regulations under laws without congressional approval. The Chevron doctrine was in play in 2023 when the Biden administration used the Department of Education to roll out the SAVE plan without congressional approval.
James Dahle, M.D., FACEP, founder of The White Coat Investor, says PSLF has been a “game changer” for physicians, with many receiving tax-free relief for hundreds of thousands of dollars. He highlights how programs like SAVE offer unprecedented generosity, even halting loan growth during residency. “Don’t be too fatalistic,” Dahle says — today’s doctors have more repayment options than ever.
“Some of the IDR programs have been incredibly generous, [for example], this one that the Trump administration is doing its best to stamp out,” Dahle said, referring to the SAVE plan. “It was a very, very generous program. … Your debt wasn’t even going up in residency like it used to.”
“A lot of things that we felt like we could count on have been pulled out from underneath us,” Foley said. “With the Chevron doctrine going away, it kind of dismantled the power of the Department of Education’s regulations. We’re at risk of them potentially changing those IDR plans down the line.”
Foley explained that only one IDR plan is rooted in law: IBR. “Plans like PAYE, SAVE, Income-Contingent Repayment, Income-Sensitive — those are regulations that could be sued in the future, just like SAVE is being sued right now.”
The implications stretch beyond legal battles. Under the court-ordered forbearance, no new borrowers can enroll in SAVE, and existing participants are not earning credit toward PSLF or IDR forgiveness unless they switch to IBR. And while IBR remains the only IDR plan currently processing forgiveness, because Congress established it, it may not be the best option for every physician, depending on income, debt load and career path.
At the same time, House Republicans are advancing legislation to cap federal graduate student borrowing at $150,000 and remove PSLF credit for time spent in medical or dental residency. This change could dramatically increase costs for trainees at nonprofit hospitals.
Other Republican-led proposals would limit who qualifies for forgiveness based on the employer’s political or advocacy affiliations, raising further concerns about future restrictions to PSLF.
“There’s also processing risk,” Foley said. “The loan servicers can be very difficult to deal with. … A lot of our clients are in the SAVE plan, and servicers are refusing to process applications to switch to IBR right now. So months go by without any credit toward PSLF or other forgiveness options.”
In an April letter, the American Medical Association (AMA) urged the Trump administration to take action on processing delays, PSLF protections and the broader uncertainty surrounding the status of IDR plans.
“This uncertainty … has caused individuals to experience continued increases in their student loan balance due to constantly accruing interest, a lack of knowledge surrounding payment amounts, and the inability to continue to accumulate time toward loan forgiveness,” wrote James L. Madara, M.D., CEO and executive vice president of the AMA.
Madara warned that instability in PSLF could undercut physician willingness to serve in high-need areas. “If this uncertainty continues … it will impact physicians’ desire to participate and thus will decrease access to much-needed medical care for patients in underserved communities.”
With the Trump administration signaling skepticism toward large-scale loan forgiveness — and key regulatory protections under legal assault — the repayment landscape for physicians has become more uncertain than ever.
Despite that volatility and ongoing legislative upheavals, the financial principles guiding loan repayment remain stable: Physicians must maintain careful, strategic approaches tailored to their individual circumstances.
Dahle remains optimistic. “Let’s not be too fatalistic that student loans are a terrible, terrible problem out there,” he said. “In a lot of ways, a lot has been done on this, and there’s a lot of great options.”
Whether relying on PSLF, pursuing aggressive repayment or navigating long-term forgiveness strategies, ongoing vigilance to policy developments is essential. More than ever, physicians must stay informed and flexible, ready to adapt to the evolving student loan landscape that continues to shape their careers and lives.
Navigating the uncertainty of student loans
A guide for physicians
Understanding your options:
The three paths
Foley broke down the repayment landscape into three primary options, each with significant trade-offs depending on income, employment type and total debt. “To get rid of people’s student loans, they have to go through one of these three paths,” Foley said.
The first is direct payment. This includes either staying in the federal system and making full monthly payments or refinancing into a private loan and choosing a fixed timeline, typically five, 10 or 15 years. This path offers simplicity and lower total interest costs for physicians with high incomes and relatively lower loan balances.
“We always want to compare the total cost of paying it off versus the forgiveness routes,” Foley explained. If the difference is small, aggressive repayment may be the safer route.
The second option is long-term IDR with taxable forgiveness at the end. Under plans like Income-Based Repayment (IBR), Pay As You Earn (PAYE) or Saving on A Valuable Education (SAVE), monthly payments are based on income and household size, not outstanding loan balance. After 20 to 25 years of monthly payments, the remaining balance is forgiven, but the forgiven amount is treated as taxable income in the year it’s forgiven.
“If you still have a balance remaining at the end of that 20 to 25 years, they’ll say, ‘Hey, you can throw in the towel. We’re going to forgive them for you,” Foley explained, including the caveat that “if you still have $300,000 remaining at that point, they’re going to add that to your taxable income in that final year of distribution. So it’s forgiven, but it’ll look like you just made an extra $300,000 that year.”
Related Podcast episode
Tammy Schaeffer, RN, JD, principal, Plante Moran, discusses the biggest obstacles practices face when transitioning to value-based care.
A decade after the passage of the Medicare Access and CHIP Reauthorization Act (MACRA), value-based care remains more promise than practice for many independent physicians. MACRA was meant to catalyze a major shift in how doctors are paid — away from fee-for-service and toward a model that rewards quality, cost efficiency and patient outcomes. But the transition has been uneven, slow and, in some cases, frustrating.
For independent practices in particular, the past 10 years have revealed both the potential and the pitfalls of value-based care. Programs like the Merit-Based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs) were designed to reward high-performing clinicians, but many doctors report burdensome reporting requirements, opaque performance benchmarks and limited financial upside. While some practices have found success, others have opted out or remained in traditional fee-for-service models, where payments may be more predictable, even if less aligned with patient outcomes.
Meanwhile, private payers have launched their own value-based care initiatives, often with different metrics, goals, and reporting systems from Medicare. The result is a fragmented landscape in which physicians may find themselves juggling multiple sets of rules, incentives and data submissions while trying to maintain quality care for patients.
So why hasn’t value-based care taken deeper root faster? For many independent physicians, the investment in infrastructure, data analytics and staffing is simply too great without a clearer or more immediate return. Others point to a lack of standardization across payers or a disconnect between quality measures and real-world clinical impact.
Ten years after MACRA’s launch, value-based care is still overshadowed by fee-for-service. Should physicians still consider moving more toward value-based care, or has MACRA proved that it won’t work?
The promise: Building a bridge to value
MACRA introduced two primary tracks to incentivize providers toward value-based care: MIPS and APMs. MIPS was intended to help physicians — especially those unfamiliar with value-based structures — ease into the new paradigm by rewarding performance on quality reporting, cost control and clinical improvement. The eventual goal was to transition providers into Advanced APMs, which require assuming more financial risk in exchange for greater potential rewards.
“The concept of linking payment to better care is the right one,” says Mark McClellan, MD, PhD, director of the Duke-Margolis Institute for Health Policy at Duke University and former CMS director during the George W. Bush administration. “And trying to get to a more stable, predictable physician payment system is critical for helping physicians invest in new kinds of care.”
Anders Gilberg, senior vice president, government affairs, Medical Group Management Association, agreed that MACRA’s two-track framework made sense: “The idea was for physicians to gain experience through MIPS and then move into APMs and develop more APMs along the way.”
In practice, though, the transition has been difficult, largely because of the limited availability of Advanced APMs. “There aren’t enough APMs to satisfy the demand for value-based care,” says Gilberg. “If we tried to move everyone into value-based care today, we’d fall short.”
Advanced APMs offer bonus payments to encourage participation and have shown more success than MIPS at aligning payment with outcomes, particularly in larger systems. “The APM bonus has been helpful in providing some reliable support as organizations move away from fee-for-service and into arrangements that are more about focusing on people and accountabilities for total costs and better results,” McClellan says.
MIPS, meanwhile, has become a source of frustration for many physicians. Gilberg says it’s often seen as a bureaucratic reporting exercise, lacking clinical relevance and meaningful incentives. The modest bonuses — largely funded by penalties on lower-performing providers — failed to drive significant change. A key flaw was the two-year lag between performance and payment. “The incentives were too disconnected from time,” Gilberg says. “The feedback was too far after the actual delivery of care to really have a meaningful clinical outcome.”
Still, MACRA achieved some important milestones. Most notably, it repealed the deeply unpopular sustainable growth rate formula, which had created annual uncertainty around Medicare payment cuts. It also marked a cultural shift in how physicians think about care, encouraging a focus on quality and cost rather than volume. Another underappreciated success was the creation of the Physician-Focused Payment Model Technical Advisory Committee (PTAC), which gave physicians a voice in shaping new models. “That was a foundationally good idea,” Gilberg says, although he noted that CMS rarely acted on PTAC’s recommendations, frustrating committee members and limiting its impact.
The value-based care train is leaving the station. Should you be on it?
Sean Cavanaugh, a former CMS deputy director under the Obama administration and now chief policy officer at Aledade, which helps primary care practices succeed in value-based care, emphasized that the broader move toward value-based care is no longer up for debate. “I don’t know a single payer or program that wants to pay anyone except on the basis of value,” says Cavanaugh. “There is still some experimenting to figure out what the right payment model is, but the argument is over; it’s now about the details.”
Public programs are already covering 13 million people through models like the Medicare Shared Savings Program, and the evidence shows they’re achieving better care at lower cost.
On the commercial side, private insurers have moved rapidly into value-based Medicare Advantage contracts, though recent challenges have made them more cautious. “Everyone’s fully committed,” Cavanaugh says. “It’s now about getting the details right. In Medicare, many early adopters joined, but we need new strategies to reach more risk-averse, mainstream providers. Fee-for-service has failed primary care, and we need different strategies to reach them.”
Medicare Advantage may end up being the primary catalyst in moving more doctors to value-based care contracts.
“More beneficiaries are now in Medicare Advantage than in traditional Medicare,” Gilberg says. “That’s important because many large medical groups run their own Medicare Advantage plans and can more easily implement value-based care within that structure.”
With full control over the care delivery and payment system — including hospitals and practices — these organizations can justify up-front investments in things like nurse navigators or remote monitoring — investments often needed for value-based care success — knowing they will reap the long-term savings.
Some issues with current models still need work, including improving cash flow, reducing administrative burden, and adjusting incentives. “If we fix those, we’ll see more primary care doctors on the sidelines decide to participate,” Cavanaugh says.
Participation in value-based care is growing overall, even if the comfort level of many physicians lies in fee-for-service arrangements. “In 2013, there were 100,000 providers in these value-based models; in 2023, nearly a quarter of a million, so that’s huge growth in provider participation,” says Emily Brower, CEO, National Association of Accountable Care Organizations (ACOs). “And now we have 56% of traditional Medicare beneficiaries attributed to ACOs. Not all of those are in Advanced Alternative Payment Models, but it has created a pathway with incentives for more providers to participate in models and then be rewarded when they move into tracks or models that have total cost of care accountability with downside risk.”
A decade of value-based care
What’s worked, what hasn’t, and how to prepare for what comes next
Still, challenges remain. Rural providers, critical access hospitals, federally qualified health centers—those that are paid differently—are harder to reach. “But even in those communities, we’re seeing growth,” Brower says.
Fee-for-service may still account for the majority of payments, and the uptake of value-based care has been slower than some experts predicted, but Tammy Schaeffer, JD, RN, principal at consulting firm Plante Moran, says that’s partly because physicians in recent history have been incentivized on volume. “Organizations have put a lot of emphasis and a lot of infrastructure behind succeeding in a fee-for-service environment,” she says. “The simple reality is that’s not all undone overnight. It’s a complete unwinding of the way that we’ve done things for the last 100 years.”
Looking ahead: Will value-based care succeed?
The future of value-based care may lie less in government-run programs like MIPS and more in market-driven models through Medicare Advantage and private insurers. But even the private sector has limitations. Gilberg notes that private payers have largely focused on primary care and population health, leaving specialty care and procedural episodes mostly on the sidelines, at least for now.
Economic realities also present challenges. Preventive care is often touted as a cost-saving measure, yet Gilberg highlights a paradox for taxpayers: “You can delay chronic conditions from developing at age 75 until 85, which is great for families and society, but you don’t necessarily see the savings the government may look for.”
McClellan says the system also carries substantial administrative burden, even for practices in Alternative Payment Models. “They still have to submit all the claims,” he says. “For most clinicians, it’s not yet turned out to be a pathway away from all of that paperwork.”
McClellan says a major obstacle is that Medicare continues to rely on fee-for-service-style diagnosis coding for risk adjustment, especially in Medicare Advantage.
“We have electronic health records widely adopted. We have interoperability standards. This should make it possible to just get the relevant clinical information on a patient’s risk from physicians’ care systems and not have to recreate fee-for-service steps in the payment process,” he says. “That’s just a big underlying mismatch that’s leading to higher costs.”
Value-based care ultimately represents a return to the roots of why many physicians chose medicine in the first place: to care for people, not just treat patients episodically. It’s a shift from reactive care — waiting to see who walks through the door — to proactive, population-based care that monitors patients outside the office, helps avoid hospitalizations and manages chronic conditions. That’s a key promise of ACOs, especially for primary care.
Three keys to succeeding in value-based care
Transitioning to value-based care can be a complicated and seemingly overwhelming task for a practice moving from fee-for-service contracts. Tammy Schaeffer, JD, RN, principal at consulting firm Plante Moran, recommends exploring upside-only risk arrangements — where the practice can earn a bonus but not be penalized — at first, giving practices time to adapt without immediate downside exposure. Once you are in value-based care, here are the three keys to success:
CLICK to Reveal
“Accessibility is the No. 1 leading indicator to success in value-based care,” she says. Practices must ensure they can see patients promptly and manage those with chronic conditions at the right frequency to avoid costly acute care. That includes understanding how quickly patients can get an appointment, how well the practice is managing complex cases and what kind of population it serves, whether that’s older adults, younger families or patients in urban areas who may have higher rates of certain comorbidities.
Step 1: Assess the practice’s current state, particularly around access.
Time to read: 8 - 9 minutes
Elements in this feature
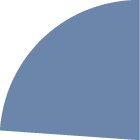
Thirty percent of organizations reported that 25% or more of their revenue is tied to value-based care contracts.


More than 60% of organizations have increased their participation in value-based programs.
To perform better in value-based care, health care organizations are investing as follows:
Source: Innovaccer/National Association of Accountable Care Organizations: The State and Science of Value Based Care 2025
Data analytics and AI.


50%
Care management technologies.


48%
Patient engagement solutions.


33%
July/August 2025
Medical Economics Insider
Anders Gilberg, senior vice president, government affairs, Medical Group Management Association, talks about whether small independent practices can survive as more payers embrace value-based care.
VBC-video-2
VBC-video-TOC
VBC- Three keys MSO
VBC- Data

Scroll to Read
Yet this shift isn’t easy for small practices. Many lack the negotiating power to secure favorable contracts and often just accept a fee schedule handed down by payers. “It is getting harder and harder for small practices to survive on their own,” Cavanaugh says. “ACOs can offer a viable pathway, but you need thousands of lives to make it viable.”
Still, as these organizations in value-based care mature, they face new hurdles. “Most have harvested the low-hanging fruit — preventive care, chronic care management, managing post-acute episodes,” says Brower. “Now they need to get more sophisticated in how they either partner with others for episodes of care or have other parts of a delivery enterprise where they can bring care to the home.”
As practices improve, they may need to look for opportunities that require greater critical mass than one practice may have on its own, says Brower. For example, there may not be enough dialysis patients for the practice to be effective or enough data analysis expertise to identify the savings opportunities. “That’s where groups will partner with others who can bring those additional tools to create that critical mass among a shared group of providers to be able to get to that next tranche of opportunity.”
The transition can be particularly complex for small physician practices. “There’s no such thing as having a fully value-based platform,” says Schaeffer. “Especially for smaller physician practices, they don’t have the luxury of saying, ‘We are going all in on value.’ They have to keep one foot in the fee-for-service canoe and one foot in the value-based care canoe. That can create extraordinarily difficult situations for them because working toward one can actually shoot them in the foot of the other.”
Yet Schaeffer sees value-based care as a way to finally reward physicians for what they’ve always tried to do: help difficult, complex patients stay healthy. “It’s the first system that really rewards all of the things that they’ve been doing all along to keep patients healthy, but appropriately aligns reimbursement with the great outcomes that they’re delivering as a result of all that work.”
As Medicare Advantage grows and private payers continue experimenting, the MACRA goal of value-based care may still come to life, just not as policymakers originally imagined.
“I really doubt that top-down mandatory programs coming out of the Centers for Medicare and Medicaid Innovation are going to save the concept of value-based care,” says Gilberg. “The only way it’s going to happen is bottom up through doctors who are delivering care every day and developing measures that are clinically relevant, that really help them improve quality. The more clinically relevant and the less financially punitive these programs are, I think the more successful they’ll be.”
Value-based care: By the numbers


Tammy Schaeffer, RN, JD, principal, Plante Moran, discusses the biggest obstacles practices face when transitioning to value-based care.
Anders Gilberg, senior vice president, government affairs, Medical Group Management Association, talks about whether small independent practices can survive as more payers embrace value-based care.
A decade after the passage of the Medicare Access and CHIP Reauthorization Act (MACRA), value-based care remains more promise than practice for many independent physicians. MACRA was meant to catalyze a major shift in how doctors are paid — away from fee-for-service and toward a model that rewards quality, cost efficiency and patient outcomes. But the transition has been uneven, slow and, in some cases, frustrating.
For independent practices in particular, the past 10 years have revealed both the potential and the pitfalls of value-based care. Programs like the Merit-Based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs) were designed to reward high-performing clinicians, but many doctors report burdensome reporting requirements, opaque performance benchmarks and limited financial upside. While some practices have found success, others have opted out or remained in traditional fee-for-service models, where payments may be more predictable, even if less aligned with patient outcomes.
Meanwhile, private payers have launched their own value-based care initiatives, often with different metrics, goals, and reporting systems from Medicare. The result is a fragmented landscape in which physicians may find themselves juggling multiple sets of rules, incentives and data submissions while trying to maintain quality care for patients.
So why hasn’t value-based care taken deeper root faster? For many independent physicians, the investment in infrastructure, data analytics and staffing is simply too great without a clearer or more immediate return. Others point to a lack of standardization across payers or a disconnect between quality measures and real-world clinical impact.
Ten years after MACRA’s launch, value-based care is still overshadowed by fee-for-service. Should physicians still consider moving more toward value-based care, or has MACRA proved that it won’t work?
By
The promise: Building a bridge
to value
MACRA introduced two primary tracks to incentivize providers toward value-based care: MIPS and APMs. MIPS was intended to help physicians — especially those unfamiliar with value-based structures — ease into the new paradigm by rewarding performance on quality reporting, cost control and clinical improvement. The eventual goal was to transition providers into Advanced APMs, which require assuming more financial risk in exchange for greater potential rewards.
“The concept of linking payment to better care is the right one,” says Mark McClellan, MD, PhD, director of the Duke-Margolis Institute for Health Policy at Duke University and former CMS director during the George W. Bush administration. “And trying to get to a more stable, predictable physician payment system is critical for helping physicians invest in new kinds of care.”
Anders Gilberg, senior vice president, government affairs, Medical Group Management Association, agreed that MACRA’s two-track framework made sense: “The idea was for physicians to gain experience through MIPS and then move into APMs and develop more APMs along the way.”
In practice, though, the transition has been difficult, largely because of the limited availability of Advanced APMs. “There aren’t enough APMs to satisfy the demand for value-based care,” says Gilberg. “If we tried to move everyone into value-based care today, we’d fall short.”
Advanced APMs offer bonus payments to encourage participation and have shown more success than MIPS at aligning payment with outcomes, particularly in larger systems. “The APM bonus has been helpful in providing some reliable support as organizations move away from fee-for-service and into arrangements that are more about focusing on people and accountabilities for total costs and better results,” McClellan says.
MIPS, meanwhile, has become a source of frustration for many physicians. Gilberg says it’s often seen as a bureaucratic reporting exercise, lacking clinical relevance and meaningful incentives. The modest bonuses — largely funded by penalties on lower-performing providers — failed to drive significant change. A key flaw was the two-year lag between performance and payment. “The incentives were too disconnected from time,” Gilberg says. “The feedback was too far after the actual delivery of care to really have a meaningful clinical outcome.”
Still, MACRA achieved some important milestones. Most notably, it repealed the deeply unpopular sustainable growth rate formula, which had created annual uncertainty around Medicare payment cuts. It also marked a cultural shift in how physicians think about care, encouraging a focus on quality and cost rather than volume. Another underappreciated success was the creation of the Physician-Focused Payment Model Technical Advisory Committee (PTAC), which gave physicians a voice in shaping new models. “That was a foundationally good idea,” Gilberg says, although he noted that CMS rarely acted on PTAC’s recommendations, frustrating committee members and limiting its impact.
The value-based care train is leaving the station. Should you be on it?
Sean Cavanaugh, a former CMS deputy director under the Obama administration and now chief policy officer at Aledade, which helps primary care practices succeed in value-based care, emphasized that the broader move toward value-based care is no longer up for debate. “I don’t know a single payer or program that wants to pay anyone except on the basis of value,” says Cavanaugh. “There is still some experimenting to figure out what the right payment model is, but the argument is over; it’s now about the details.”
Public programs are already covering 13 million people through models like the Medicare Shared Savings Program, and the evidence shows they’re achieving better care at lower cost.
On the commercial side, private insurers have moved rapidly into value-based Medicare Advantage contracts, though recent challenges have made them more cautious. “Everyone’s fully committed,” Cavanaugh says. “It’s now about getting the details right. In Medicare, many early adopters joined, but we need new strategies to reach more risk-averse, mainstream providers. Fee-for-service has failed primary care, and we need different strategies to reach them.”
Medicare Advantage may end up being the primary catalyst in moving more doctors to value-based care contracts.
“More beneficiaries are now in Medicare Advantage than in traditional Medicare,” Gilberg says. “That’s important because many large medical groups run their own Medicare Advantage plans and can more easily implement value-based care within that structure.”
With full control over the care delivery and payment system — including hospitals and practices — these organizations can justify up-front investments in things like nurse navigators or remote monitoring — investments often needed for value-based care success — knowing they will reap the long-term savings.
Some issues with current models still need work, including improving cash flow, reducing administrative burden, and adjusting incentives. “If we fix those, we’ll see more primary care doctors on the sidelines decide to participate,” Cavanaugh says.
Participation in value-based care is growing overall, even if the comfort level of many physicians lies in fee-for-service arrangements. “In 2013, there were 100,000 providers in these value-based models; in 2023, nearly a quarter of a million, so that’s huge growth in provider participation,” says Emily Brower, CEO, National Association of Accountable Care Organizations (ACOs). “And now we have 56% of traditional Medicare beneficiaries attributed to ACOs. Not all of those are in Advanced Alternative Payment Models, but it has created a pathway with incentives for more providers to participate in models and then be rewarded when they move into tracks or models that have total cost of care accountability with downside risk.”
Still, challenges remain. Rural providers, critical access hospitals, federally qualified health centers—those that are paid differently—are harder to reach. “But even in those communities, we’re seeing growth,” Brower says.
Fee-for-service may still account for the majority of payments, and the uptake of value-based care has been slower than some experts predicted, but Tammy Schaeffer, JD, RN, principal at consulting firm Plante Moran, says that’s partly because physicians in recent history have been incentivized on volume. “Organizations have put a lot of emphasis and a lot of infrastructure behind succeeding in a fee-for-service environment,” she says. “The simple reality is that’s not all undone overnight. It’s a complete unwinding of the way that we’ve done things for the last 100 years.”
A decade of value-based care
What’s worked,
what hasn’t,
and how to prepare
for what comes next
Looking ahead: Will value-based care succeed?
The future of value-based care may lie less in government-run programs like MIPS and more in market-driven models through Medicare Advantage and private insurers. But even the private sector has limitations. Gilberg notes that private payers have largely focused on primary care and population health, leaving specialty care and procedural episodes mostly on the sidelines, at least for now.
Economic realities also present challenges. Preventive care is often touted as a cost-saving measure, yet Gilberg highlights a paradox for taxpayers: “You can delay chronic conditions from developing at age 75 until 85, which is great for families and society, but you don’t necessarily see the savings the government may look for.”
McClellan says the system also carries substantial administrative burden, even for practices in Alternative Payment Models. “They still have to submit all the claims,” he says. “For most clinicians, it’s not yet turned out to be a pathway away from all of that paperwork.”
McClellan says a major obstacle is that Medicare continues to rely on fee-for-service-style diagnosis coding for risk adjustment, especially in Medicare Advantage.
“We have electronic health records widely adopted. We have interoperability standards. This should make it possible to just get the relevant clinical information on a patient’s risk from physicians’ care systems and not have to recreate fee-for-service steps in the payment process,” he says. “That’s just a big underlying mismatch that’s leading to higher costs.”
Value-based care ultimately represents a return to the roots of why many physicians chose medicine in the first place: to care for people, not just treat patients episodically. It’s a shift from reactive care — waiting to see who walks through the door — to proactive, population-based care that monitors patients outside the office, helps avoid hospitalizations and manages chronic conditions. That’s a key promise of ACOs, especially for primary care.
Yet this shift isn’t easy for small practices. Many lack the negotiating power to secure favorable contracts and often just accept a fee schedule handed down by payers. “It is getting harder and harder for small practices to survive on their own,” Cavanaugh says. “ACOs can offer a viable pathway, but you need thousands of lives to make it viable.”
Still, as these organizations in value-based care mature, they face new hurdles. “Most have harvested the low-hanging fruit — preventive care, chronic care management, managing post-acute episodes,” says Brower. “Now they need to get more sophisticated in how they either partner with others for episodes of care or have other parts of a delivery enterprise where they can bring care to the home.”
As practices improve, they may need to look for opportunities that require greater critical mass than one practice may have on its own, says Brower. For example, there may not be enough dialysis patients for the practice to be effective or enough data analysis expertise to identify the savings opportunities. “That’s where groups will partner with others who can bring those additional tools to create that critical mass among a shared group of providers to be able to get to that next tranche of opportunity.”
The transition can be particularly complex for small physician practices. “There’s no such thing as having a fully value-based platform,” says Schaeffer. “Especially for smaller physician practices, they don’t have the luxury of saying, ‘We are going all in on value.’ They have to keep one foot in the fee-for-service canoe and one foot in the value-based care canoe. That can create extraordinarily difficult situations for them because working toward one can actually shoot them in the foot of the other.”
Yet Schaeffer sees value-based care as a way to finally reward physicians for what they’ve always tried to do: help difficult, complex patients stay healthy. “It’s the first system that really rewards all of the things that they’ve been doing all along to keep patients healthy, but appropriately aligns reimbursement with the great outcomes that they’re delivering as a result of all that work.”
As Medicare Advantage grows and private payers continue experimenting, the MACRA goal of value-based care may still come to life, just not as policymakers originally imagined.
“I really doubt that top-down mandatory programs coming out of the Centers for Medicare and Medicaid Innovation are going to save the concept of value-based care,” says Gilberg. “The only way it’s going to happen is bottom up through doctors who are delivering care every day and developing measures that are clinically relevant, that really help them improve quality. The more clinically relevant and the less financially punitive these programs are, I think the more successful they’ll be.”
Three keys to succeeding
in value-based care
Transitioning to value-based care can be a complicated and seemingly overwhelming task for a practice moving from fee-for-service contracts. Tammy Schaeffer, JD, RN, principal at consulting firm Plante Moran, recommends exploring upside-only risk arrangements — where the practice can earn a bonus but not be penalized — at first, giving practices time to adapt without immediate downside exposure. Once you are in value-based care, here are the three keys to success:
TAP to Reveal
Time to read: 8 - 9 minutes
“Accessibility is the No. 1 leading indicator to success in value-based care,” she says. Practices must ensure they can see patients promptly and manage those with chronic conditions at the right frequency to avoid costly acute care. That includes understanding how quickly patients can get an appointment, how well the practice is managing complex cases and what kind of population it serves, whether that’s older adults, younger families or patients in urban areas who may have higher rates of certain comorbidities.
Step 1: Assess the practice’s current state, particularly around access.
Thirty percent of organizations reported that 25% or more of their revenue is tied to value-based care contracts.


More than 60% of organizations have increased their participation in value-based programs.
To perform better in value-based care, health care organizations are investing as follows:
Source: Innovaccer/National Association of Accountable Care Organizations: The State and Science of Value Based Care 2025
Data analytics and AI.


50%
Care management technologies.


48%
Patient engagement solutions.


33%
The 2025 Physician Report
An early look at hot-button topics
The Medical Economics Physician Report is a 96-year-old survey where we break down all the most pressing issues facing physicians, including salary, practice financial health, malpractice costs, productivity and more.
This year, we asked a few new questions on hot-button topics, which we’ll share exclusively in MedEc Insider. Check out the July/August print issue of Medical Economics for the full results of the 2025 Physician Report.
Primary care physician pay
Do you believe primary care physicians (family medicine, internal medicine, pediatrics, etc) are underpaid?
Federal health policy
The Trump administration has made many changes to federal government health agencies. What do you think about these moves when it comes to practicing medicine in the U.S.?
Malpractice fears
Do you worry about being sued for malpractice?
Prior authorizations
In your practice’s experience, are prior authorization burdens getting better or worse?
Better: 1%
Artificial intelligence
Does your practice use AI tools for specific business purposes?
Top places AI helped:
No: 6%
Not sure: 2%



They will help physicians practice medicine: 17%
They will hinder physicians from practicing medicine: 61%
They will have no effect: 22%


Yes: 92%
Yes: 24%
No: 76%
Yes: 62%
Administrative tasks
Data reporting and analytics
Documentation/scribing
No: 38%
About the same: 31%
Worse: 68%
July/August 2025
Medical Economics Insider



The Medical Economics Physician Report is a 96-year-old survey where we break down all the most pressing issues facing physicians, including salary, practice financial health, malpractice costs, productivity and more.
This year, we asked a few new questions on hot-button topics, which we’ll share exclusively in MedEc Insider. Check out the July/August print issue of Medical Economics for the full results of the 2025 Physician Report.
The 2025 Physician Report
An early look at hot-button topics
Primary care physician pay
Do you believe primary care physicians (family medicine, internal medicine, pediatrics, etc) are underpaid?
Federal health policy
The Trump administration has made many changes to federal government health agencies. What do you think about these moves when it comes to practicing medicine in the U.S.?
No: 6%
Not sure: 2%


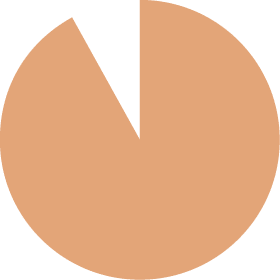
Yes: 92%
They will help physicians practice medicine: 17%
They will hinder physicians from practicing medicine: 61%
They will have no effect: 22%
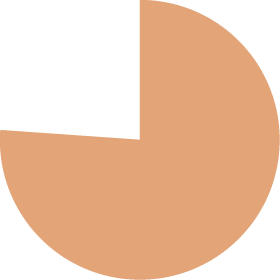
Yes: 24%
No: 76%
Artificial intelligence
Does your practice use AI tools for specific business purposes?
Top places AI helped:
Administrative tasks
Data reporting and analytics
Documentation/scribing
Prior authorizations
In your practice’s experience, are prior authorization burdens getting better or worse?
Better: 1%


About the same: 31%
Worse:
68%
Malpractice fears
Do you worry about being sued for malpractice?


Yes: 62%
No: 38%

12 steps to nail level-of-care coding
and guard against audits
A single under-documented office visit can trigger weeks of payer scrutiny and thousands in lost revenue. Yet over-coding without solid back-up invites the equal-and-opposite pain of claw-backs and potential fraud exposure. The following quick-hit checklist distills 2025 Evaluation-and-Management rules into 12 practical moves any outpatient practice can weave into its daily workflow. Use it as a living reference to ensure each note tells the full clinical story, supports the chosen CPT level, and captures every dollar your care has earned.
July/August 2025
Medical Economics Insider

12 steps to nail level-of-care coding and guard against audits
A single under-documented office visit can trigger weeks of payer scrutiny and thousands in lost revenue. Yet over-coding without solid back-up invites the equal-and-opposite pain of claw-backs and potential fraud exposure. The following quick-hit checklist distills 2025 Evaluation-and-Management rules into 12 practical moves any outpatient practice can weave into its daily workflow. Use it as a living reference to ensure each note tells the full clinical story, supports the chosen CPT level, and captures every dollar your care has earned.
What to do: Use this checklist to catch trends early: MDM documented? Time stated? Diagnosis ↔ plan match? Modifier justified? Clean claims = faster cash.
What to do: When notes are thin or illegible, query the clinician immediately rather than guessing; it’s the fastest way to cut re-work.
What to do: Code to the highest supported specificity—no more, no less. Both over- and under-coding invite audits and claw-backs.
What to do: CPT/E/M rules shift every year; outdated grids lead to instant denials. Schedule a quick staff huddle each January.
What to do: Simple mis-keyed E/M levels are top audit triggers—build an end-of-day checklist or EHR rule to flag mismatches.
What to do: Bullet “Rx management with chronic anticoagulant” or “Decision for hospital admit” to prove moderate- or high-risk MDM.
What to do: Separate preventive visits, procedures or same-day surgeries with a distinct note section; then append the modifier to show independent work and safeguard payment.
What to do: Briefly reference prior issues and give a clear return-interval (“re-check BP in 2 wks”). It demonstrates ongoing complexity and supports higher levels when warranted.
What to do: Document only what’s relevant, but be sure the history, exam, and MDM story all line up so the code looks inevitable to an auditor.
What to do: Sum all qualifying work on the date of service—pre-visit record review, face-to-face work, and same-day documentation/care coordination. Note the minutes right in the note header.
What to do: Choose the level after you’ve documented the number/complexity of problems, data reviewed, and risk. MDM is now the primary driver of 99202-99215 selection.
What to do: Auditors expect working diagnoses consistent with findings and plans. A one-line assessment (“Bacterial sinusitis—ordering CT to r/o abscess”) nails medical necessity.
Step 12
Self-audit 10 charts a month
Step 11
Cultivate coder-provider communication
Step 10
Reject up-/down-coding and unbundling
Step 9
Stay current—update cheat sheets annually
Step 8
Double-check codes before submission
Step 7
Document risk in the note, not just your head
Step 6
Use modifiers 25, 24, 57 correctly
Step 5
Address unresolved problems and spell out follow-up
Step 3
Make history and exam clinically necessary—and consistent
Step 2
Record total provider time (only when time is your basis)
Step 1
Lead with Medical Decision Making (MDM)
Step 4
Tie every order or treatment to a diagnosis statement
Editorial
Senior Vice President, Content Allie Karas, MA
Vice President, Content Chris Mazzolini, MS
cmazzolini@mjhlifesciences.com
Managing Editor Todd Shryock
tshryock@mjhlifesciences.com
Senior Editor Richard Payerchin
rpayerchin@mjhlifesciences.com
Assistant Editor Austin Littrell
alittrell@mjhlifesciences.com
Design
Creative Director Robert McGarr
Copyediting
Vice President, Copy Jennifer Potash
Copy Chief Paul Silverman
Copy Director Nicole Canfora Lupo
Copy Supervisors Angie DeRosa
Senior Copy Editors Cheney Baltz, Marie-Louise Best, Kathy Hayes,
Kelly King, Kim Nir
Substantive Editor Georgina Carson
Copy Editor Kristy Mackay
Publishing & Sales
Executive Vice President Brian Haug
Business Development
Jeffrey Chase, Vincent Maglione, Emily Rosenthal
Account Manager, Recruitment Joanna Shippoli
Executive Assistant Brielle Eder
Corporate
Chairman & CEO Mike Hennessy Jr.
Chief Financial Officer Neil Glasser, CPA/CFE
Chief Operating Officer Beth Buehler
Chief Brand Officer Silas Inman
Chief Data Officer Terric Townsend
Executive Vice President, Global Medical Affairs
& Corporate Development Joe Petroziello
Senior Vice President, Human Resources
& Administration Shari Lundenberg
Senior Vice President, Mergers & Acquisitions,
Strategic Innovation Phil Talamo
Executive Creative Director Jeff Brown
Founder Mike Hennessy Sr., 1960-2021
© 2025 MultiMedia Medical LLC All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical including by photocopy, recording, or information storage and retrieval without permission in writing from the publisher. Authorization to photocopy items for internal/educational or personal use, or the internal/educational or personal use of specific clients is granted by MultiMedia Medical LLC for libraries and other users registered with the Copyright Clearance Center, 222 Rosewood Dr. Danvers, MA 01923, 978-750-8400 fax 978-646-8700 or visit http://www.copyright.com online.
MJH Life Sciences® provides certain customer contact data (such as customers name, addresses, phone numbers, and e-mail addresses) to third parties who wish to promote relevant products, services, and other opportunities that may be of interest to you. If you do not want MJH Life Sciences to make your contact information available to third parties for marketing purposes, simply call toll-free 866-529-2922 between the hours of 7:30 a.m. and 5 p.m. CST and a customer service representative will assist you in removing your name from MJH Life Sciences lists. Outside the US, please phone 218-740-6477.
Medical Economics does not verify any claims or other information appearing in any of the advertisements contained in the publication and cannot take responsibility for any losses or other damages incurred by readers in reliance of such content.
Medical Economics cannot be held responsible for the safekeeping or return of unsolicited articles, manuscripts, photographs, illustrations, or other materials.
To subscribe, call (609) 716-7777 or email customerservice@mjhlifesciences.com.
About us















July/August 2025
Medical Economics Insider
Editorial
Senior Vice President, Content Allie Karas, MA
Vice President, Content Chris Mazzolini, MS
cmazzolini@mjhlifesciences.com
Managing Editor Todd Shryock
tshryock@mjhlifesciences.com
Senior Editor Richard Payerchin
rpayerchin@mjhlifesciences.com
Assistant Editor Austin Littrell
alittrell@mjhlifesciences.com
Design
Creative Director Robert McGarr
Copyediting
Vice President, Copy Jennifer Potash
Copy Chief Paul Silverman
Copy Director Nicole Canfora Lupo
Copy Supervisors Angie DeRosa
Senior Copy Editors Cheney Baltz, Marie-Louise Best, Kathy Hayes,
Kelly King, Kim Nir
Substantive Editor Georgina Carson
Copy Editor Kristy Mackay
Publishing & Sales
Executive Vice President Brian Haug
Business Development
Jeffrey Chase, Vincent Maglione, Emily Rosenthal
Account Manager, Recruitment Joanna Shippoli
Executive Assistant Brielle Eder
Corporate
Chairman & CEO Mike Hennessy Jr.
Chief Financial Officer Neil Glasser, CPA/CFE
Chief Operating Officer Beth Buehler
Chief Brand Officer Silas Inman
Chief Data Officer Terric Townsend
Executive Vice President, Global Medical Affairs
& Corporate Development Joe Petroziello
Senior Vice President, Human Resources
& Administration Shari Lundenberg
Senior Vice President, Mergers & Acquisitions,
Strategic Innovation Phil Talamo
Executive Creative Director Jeff Brown
Founder Mike Hennessy Sr., 1960-2021
© 2025 MultiMedia Medical LLC All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical including by photocopy, recording, or information storage and retrieval without permission in writing from the publisher. Authorization to photocopy items for internal/educational or personal use, or the internal/educational or personal use of specific clients is granted by MultiMedia Medical LLC for libraries and other users registered with the Copyright Clearance Center, 222 Rosewood Dr. Danvers, MA 01923, 978-750-8400 fax 978-646-8700 or visit http://www.copyright.com online.
MJH Life Sciences® provides certain customer contact data (such as customers name, addresses, phone numbers, and e-mail addresses) to third parties who wish to promote relevant products, services, and other opportunities that may be of interest to you. If you do not want MJH Life Sciences to make your contact information available to third parties for marketing purposes, simply call toll-free 866-529-2922 between the hours of 7:30 a.m. and 5 p.m. CST and a customer service representative will assist you in removing your name from MJH Life Sciences lists. Outside the US, please phone 218-740-6477.
Medical Economics does not verify any claims or other information appearing in any of the advertisements contained in the publication and cannot take responsibility for any losses or other damages incurred by readers in reliance of such content.
Medical Economics cannot be held responsible for the safekeeping or return of unsolicited articles, manuscripts, photographs, illustrations, or other materials.
To subscribe, call (609) 716-7777 or email customerservice@mjhlifesciences.com.
About us














